Common Containment Challenges on Active Healthcare Job Sites
A practical perspective informed by ICRA 2.0, ASHE, and real-world construction conditions
Containment is a foundational requirement in healthcare construction. Its purpose is simple but critical: prevent the migration of dust, debris, and airborne contaminants from construction areas into occupied clinical spaces.
ICRA or ICRA 2.0 by ASHE provide guidance on containment classifications, pressure relationships, and required controls. However, the greatest challenges do not often occur during planning or initial setup, they emerge during active construction, when job sites are constantly changing.
Understanding where containment commonly breaks down helps teams design systems that are not only compliant on paper, but resilient in practice.
Why Containment Is More Challenging on Active Job Sites
Unlike new construction, healthcare renovation and infrastructure projects occur within fully operational facilities. Clinical activity continues, HVAC systems serve adjacent spaces, and multiple stakeholders interact with containment systems daily. In this environment, containment is not a static installation. It is an active control system that must adapt to changing conditions while maintaining consistent performance.
1. Static Containment Plans in a Dynamic Environment
Containment strategies are usually defined during preconstruction meetings, where the ICRA plan is created and key details, machine quantities, pressure monitoring, temporary wall locations, and exhaust airflow access, are determined. But in reality:
- Work phases overlap or change
- Temporary walls are moved
- Ceiling access and penetration evolve
- Adjacent spaces change use
Containment plans are rarely updated at the same pace as job-site changes. Over time, assumptions made during planning no longer reflect site conditions, increasing the risk of unrecognized containment gaps.
2. Negative pressure is difficult to consistently maintain
Initial containment setup often includes smoke testing and negative air machine validation to confirm pressure relationships. While these checks may pass at setup, maintaining stable negative pressure over time is significantly more challenging. Common causes of pressure loss include:
- Frequent door openings
- Negative air machine filter loading over time
- HVAC mode changes in adjacent spaces
- Power interruptions or equipment downtime
Pressure loss often occurs between manual checks. Short-duration failures or gradual degradation may go unnoticed, even though containment effectiveness is temporarily compromised.
3. Managing pressure with barriers
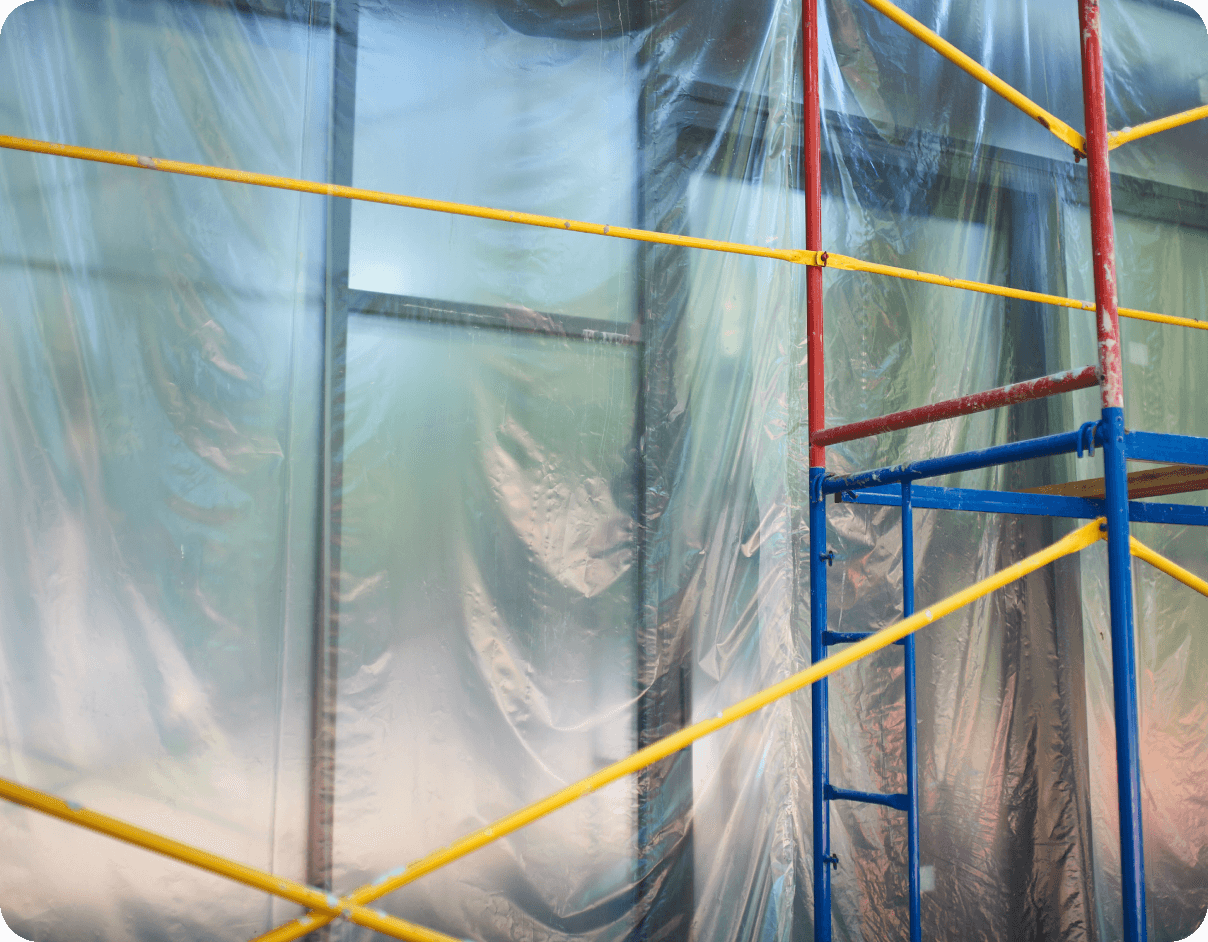
The most common barrier types used on healthcare construction sites include temporary hard walls, plastic barriers, and zipper doors. As hospitals increase restrictions on plastic barriers, many projects are shifting toward hard-wall containment due to improved durability and pressure stability. Typical issues include:
- Gaps at wall-to-ceiling interfaces
- Excessive negative pressure pulling down plastic barriers
- Interaction with adjacent return air pathways
- Unsealed penetrations for utilities or cabling
Visual containment does not guarantee airflow containment. Barriers that appear intact may still allow airborne contaminants to migrate if pressure relationships and leakage paths are not properly controlled and verified.
4. Door usage and human factors
Containment relies heavily on controlled access points, including anterooms and door sequencing. However, active job sites introduce unavoidable human variability. Common pitfalls:
- Material and equipment moving in & out
- Multiple trades share the same access points
- Clinical staff may pass through containment areas
- Equipment being removed or stolen from job sites
Even brief or unintended door misuse can disrupt pressure relationships. Containment strategies that depend on perfect human behavior are inherently fragile. Effective containment systems must account for real-world usage, not ideal conditions.
5. Limited Visibility Into Containment Performance
Containment effectiveness depends on maintaining pressure relationships over time. However, on active healthcare job sites, visibility into ongoing performance is often limited to periodic checks, analog systems, and manual observation. Common realities include:
- Pressure drop alarm being missed
- Time spent reconstructing what happened and when
- Increasing documentation requirements from hospitals
- Project delays due to equipment planning or availability
Containment strategies that rely on intermittent visibility are inherently fragile. Effective containment requires continuous awareness that aligns with how healthcare job sites operate, across shifts, evolving scopes, and changing site conditions.

Containment challenges on active healthcare job sites are rarely caused by a single failure. They result from dynamic environments, human factors, and limited visibility into ongoing performance.
ICRA 2.0 guideline defines what effective containment should achieve. The challenge in practice is maintaining that effectiveness throughout the life of an active project. Containment systems designed for adaptability, continuous verification, and real-world workflows are far more resilient than those built solely around initial setup and periodic checks.